Getting Hyper-Fixated on Hypothyroidism
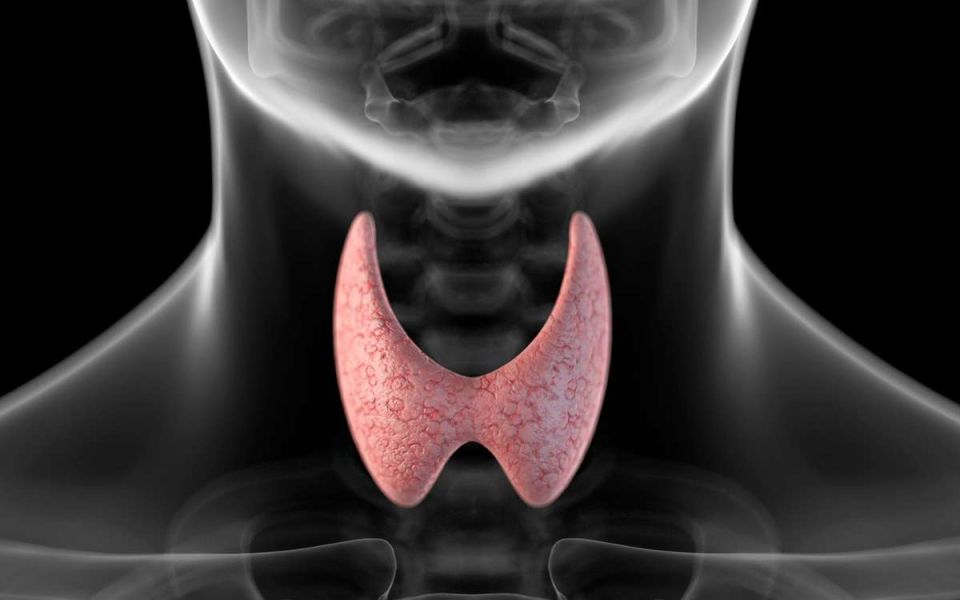
The body is as amazing as it is complex. Consider the thyroid, this tiny gland sits in your neck, just under the Adam’s apple (larynx), and is butterfly-shaped (technically, thyroid comes from the Greek word for an oblong shield, but it’s butterfly season, and I haven’t used a Greek shield in a hot minute.) It’s unassuming, easy to miss, and affects nearly every cell in the body. The thyroid is part of the endocrine system, which is responsible for producing and releasing hormones that regulate countless bodily functions. The endocrine system is a messenger system of interwebbed feedback loops that regulate how the body metabolizes food products into energy, cellular materials, and waste. Disruptions in this system can have enormous downstream effects, as with the thyroid.
The hypothalamus-pituitary-thyroid axis
The thyroid is part of the hypothalamus-pituitary-thyroid axis. The hypothalamus is in the brain. When it senses low levels of thyroid hormones, it tells the pituitary gland (at the base of the brain) to release Thyroid-stimulating hormone (TSH). This, predictably, stimulates the thyroid to produce more hormones. Doctors monitor TSH levels when checking on thyroid function. TSH activates the thyroid, which produces Thyroxine (tetraiodothyronine, or T4) and Triiodothyronine (T3). These names are long and complicated, but the presence of “iodo” in the middle provides a clue that iodine is a key part of these chemicals. Stay tuned for more on that later. The thyroid also produces calcitonin, which can regulate calcium levels. T4 and T3 are the hormones monitored by the hypothalamus: if it detects enough in the blood, it tells the pituitary gland to lower TSH production. Together, measuring the levels of TSH, T4, and T3 can give a good idea of how the thyroid is performing.
Surprisingly, the thyroid produces only about 20% of the body’s T3, the majority is derived from T4 which has been delivered to body tissue! You can think of T4 as a long-lasting store of T3, though it also has some effect on specific cells. T3 is a big deal, it has metabolic effects on basically all cells and promotes protein production. Strangely, 99% of all T3 and T4 are bound in proteins and unable to activate cell receptors. The unbound 1% is called free T3 (and free T4) and is what’s responsible for the metabolic effects. When the thyroid is disrupted all sorts of things can go wrong.
People who have an underproduction of thyroid hormones have hypothyroidism. Hypo- means low, or under, thyroid indicates the thyroid, and -ism means a condition of. Hypothyroidism is a condition where the thyroid underproduces hormones. Hypothyroidism affects between 2-11% of the adult US population. The primary risk factor is age, with those over sixty having higher rates of hypothyroidism. It is 20 times as prevalent in women. Worldwide, the highest cause of hypothyroidism is low iodine intake, which restricts T4 and T3 production. Here in the US we get plenty of iodine in our diets, so the highest cause here is autoimmune inflammation, a condition called Hashimoto’s disease. The next highest cause of hypothyroidism is treatment for hyperthyroidism - when the thyroid is overactive. This makes intuitive sense, as getting the balance exactly perfect is nearly impossible. In rare cases, the hypothalamus or pituitary gland may malfunction.
The causes of hypothyroidism can be widespread, and so can the effects. When tissues can’t get enough T3, all sorts of problems arise. Common symptoms include fatigue, weight gain, changes to hair and skin, sensitivity to cold, and mental changes to mood and memory. Several patients experience no symptoms, and several patients have comorbidities (such as other autoimmune inflammation), making isolating symptoms and causes difficult. Untreated hypothyroidism can lead to heart problems and swelling of the thyroid, which is called a goiter. So what can be done? Is there any hope?
It should be no surprise that the solution to hypothyroidism is to take supplemental T4 and/or T3. In ye olden days (the 1950’s) the solution to hypothyroidism was to consume dried and prepared sections of animal thyroid - which would otherwise go to waste anyway. This can still be found under several names: desiccated thyroid, thyroid extract, Armour Thyroid, Thyroid USP, natural thyroid, and more. In the 1960’s, levothyroxine - synthetic T4 - was developed. A diagnosis of hypothyroidism may include low T4 and T3 levels, along with elevated TSH. Levothyroxine has been the standard treatment since the 1960’s and can bring hormone levels back in line. Unfortunately, a significant amount of patients do not find symptomatic relief from levothyroxine. It is thought that even though T4 levels are being raised, T3 may not be reaching the tissue. Perhaps the feedback loop isn’t complete. To compensate for this, some doctors have been prescribing T3 along with levothyroxine, with mixed results. Researchers have also been studying if the past solution, animal thyroid, may be the future solution. Thyroid extract generally results in lower free T4 and more free T3. With luck (and clinical trials!) we can find solutions to keep the butterfly in our throats flying high and functioning majestically.
Staff Writer/Editor Benton Lowey-Ball, BS, BFA
Click Below for ENCORE Research Group's Enrolling Studies
References:
Biondi, B., & Wartofsky, L. (2014). Treatment with thyroid hormone. Endocrine reviews, 35(3), 433-512. https://academic.oup.com/edrv/article/35/3/433/2354656
Boucai. L., (2024). Overview of thyroid function. Merck Manual, Professional Version. https://www.merckmanuals.com/professional/endocrine-and-metabolic-disorders/thyroid-disorders/hypothyroidism
Boucai. L., (2024). Hypothyroidism. Merck Manual, Professional Version. https://www.merckmanuals.com/professional/endocrine-and-metabolic-disorders/thyroid-disorders/hypothyroidism
Hegedüs, L., Bianco, A. C., Jonklaas, J., Pearce, S. H., Weetman, A. P., & Perros, P. (2022). Primary hypothyroidism and quality of life. Nature Reviews Endocrinology, 18(4), 230-242. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8930682/
Wyne, K. L., Nair, L., Schneiderman, C. P., Pinsky, B., Antunez Flores, O., Guo, D., ... & Tessnow, A. H. (2023). Hypothyroidism prevalence in the United States: a retrospective study combining national health and nutrition examination survey and claims data, 2009–2019. Journal of the Endocrine Society, 7(1), bvac172. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9706417/